Autism Spectrum Disorder (ASD) is characterized by the presence of persistent deficits in social communication and social interaction across multiple contexts as well as restrictive, repetitive behavior, interests, or activities (American Psychiatric Association, 2013). Many individuals with ASD require some level of support for social and communication skills and to promote independence with daily tasks. Additionally, some individuals may experience behavioral excesses that interfere with learning and engagement in daily activities or pose a risk to their health and safety.

The behavioral characteristics common to ASD are also often common to, or can be complicated by, a number of developmental, medical, and psychiatric conditions. Research indicates that individuals with ASD are very likely to experience co-occurring conditions such as developmental disabilities, epilepsy, gastro-intestinal issues, sleep disruption, feeding issues, and psychiatric disorders (Autism Speaks, 2017). Knowledge of co-occurring conditions and how they may present in individuals with ASD can inform a more comprehensive, interdisciplinary approach to behavioral assessment and intervention that supports best outcomes for individuals served. Additionally, the consistent use of the strategies discussed within this article may help to identify new or undiagnosed conditions that may alter the course of ongoing intervention to best meet the needs of the individual.
Assessment in the Context of Co-Occurring Conditions
Behavioral assessment is a cornerstone of quality behavior analytic work, guiding the development of effective and meaningful interventions (e.g., Carr et al., 1994; Goldiamond, 1974). Individualized and contextualized behavioral assessment selection and design can also identify behavioral patterns that are indicative of possible co-occurring conditions, prompting interdisciplinary collaboration. Likewise, well-crafted assessments can guide existing collaborations and ultimately inform intervention development beyond a purely behavior analytic lens. Regardless if there is a known co-occurring condition, behavior analysts are ethically bound to consider and assess the role of health or other variables when assessing behavior and collaborate with relevant professionals (Behavior Analyst Certification Board, 2020; see code 2.12).
How can assessments identify behavioral patterns indicative of a co-occurring condition? Tools and assessments that can guide this process might include a thorough review of client records, surveys completed by caregivers or others familiar with the individual, direct observations, plotting behavioral data across different variables (i.e., scatterplot), analyzing events immediately prior and following behavior, assessing preference, or systematically arranging specific conditions and observing behavior within them. These approaches can shed light on the behavior of interest and can be used to detect how co-occurring conditions relate, by providing more information with respect to the following:
- Does the behavior occur irrespective of context?
- When does the behavior occur in relation to other variables?
- What does the behavior look like?
If the behavior of interest persists irrespective of environmental contexts or ongoing activities, our assessment and investigative work are far from over. This does, however, inform us that there is likely a variable at play that is not captured in the immediate social environment, and some aspect of engaging in the behavior may be contributing to its persistence (i.e., automatic reinforcement; Vollmer, 1994). For instance, the individual may be responding to internal stimulation and the target behavior may be alleviating discomfort or pain, prompting further medical assessment.
With information about when the behavior occurs with respect to other variables (i.e., temporal relations), correlational information might inform us that the behavior is more or less likely to occur around particular times or activities. For instance, there might be patterns surrounding particular times of day, days of week, or times of month, corresponding to biological factors such as sleep, bowel movements, meals, menstrual cycles, seizure activity, or medication. Depending on behavioral patterns that are identified, behavior analysts can then initiate collaboration with professionals specializing in that area or areas.
Identified patterns related to medication might prompt collaboration with prescribing psychiatrists, neurologists, or physicians, helping identify paradoxical effects of medication or needed adjustments to scheduled administration times (e.g., stimulants to treat attention deficit hyperactivity disorder). Ongoing assessment throughout the collaboration will help each professional bring their expertise to the table in the design, implementation, and monitoring of interventions leading to best outcomes for the individual (e.g., Bird et al., 2022).
In addition to the contexts in which behavior is observed and the relation of its occurrence to other variables, how the behavior looks or its topography can be equally insightful. Most notably, behavior directed at a specific area of the body might be indicative of pain, discomfort, or a medical condition, prompting medical examination. As an example, you might suggest an individual who engages in persistent self-scratching is assessed by a dermatologist. Similarly, if self-injury shifts to a novel topography targeting the abdomen, seeking assessment from a gastroenterologist or gynecologist might be appropriate.
The topography, or form, of behavior can also be correlated to specific diagnoses, with syndrome groups associated with specific behavioral profiles. Several examples include Down syndrome corresponding to higher social skills ratings and lower levels of challenging behavior, Prader-Willi syndrome corresponding to higher levels of behavior characterized as anxious or repetitive, and Angelman syndrome corresponding to a demonstrably happy affect, hand-clapping, and mouthing behavior (Walz & Benson, 2002). In both assessment and intervention phases, it is important to keep behavioral profiles related to co-occurring conditions or diagnoses in mind.
At times, the forms of behavior associated with specific diagnoses are repetitive, or stereotypic, in nature, similar to what is noted for Prader-Willi syndrome as mentioned above. This can also be the case for anxiety (Moore et al., 2021), vision impairment or deaf blindness (Gal & Dyck, 2009, Molloy & Rowe, 2011, Singer et al., 2021), Obsessive Compulsive Disorder (OCD; Chok & Kesseler, 2014), among other conditions. Repetitive, or stereotypic, behavior can present in a variety of forms, such as body rocking, hand-flapping, or eye-pressing. Most often, such behavior persists irrespective of context or social consequences, suggesting it is at least partially maintained by automatic reinforcement (Rapp & Vollmer, 2005). Nonetheless, assessment can still prove to be beneficial as it can guide the identification of specific co-occurring conditions, inform intervention design, and serve as relevant information in evaluating interventions.
Intervention Considerations in the Context of Co-Occurring Conditions
Using behavioral assessment in conjunction with information specific to co-occurring conditions can enhance the efficacy of treatment (Brodhead, 2015). At times, the presence of some conditions might contraindicate behavioral intervention that would otherwise be considered best practice. For example, toilet training procedures in the face of co-occurring gastrointestinal (GI) difficulties or the treatment of vocal perseverations in the presence of a co-occurring anxiety diagnosis require consideration of the interactional effects across diagnoses. When faced with such co-occurring conditions, behavior analysts must consider if they have the expertise to serve the client. If not, consulting with other professionals or seeking additional education might be necessary.
When addressing behavior related to co-occurring conditions, it is critical that clinicians and collaborating professionals consider the following questions throughout the intervention process:
- Are there any contraindications of a function-based intervention?
- How can interdisciplinary collaboration guide intervention?
- How does the intervention take the whole person into account?
Designing Interdisciplinary Interventions
In the context of co-occurring conditions, medical, genetic, or otherwise, intervention is often multi-faceted and spans across disciplines (Cox, 2012). For example, when a behavior analyst is tasked with addressing frequent bowel movement accidents of a client with an ASD diagnosis and a GI condition, they should be asking “How can interdisciplinary collaboration guide intervention?” Consideration of both diagnoses prompts professionals to take the whole person into account during intervention development. A purely function-based approach is likely not the best option; given the GI condition, a treatment package involving both medication and behavior analytic procedures will likely be most effective. In this case, intervention might involve ongoing medication, as-needed laxatives, scheduled bathroom trips, and rewards or reinforcement for successful toileting. Assessment of both the medical components and daily patterns would inform the prescribed medication and best schedule of proactive bathroom trips. This is one of countless scenarios in which taking co-occurring conditions into account in the assessment and intervention of behavioral targets leads to best outcomes.
At times, contraindications can be addressed through direct modification of behavioral interventions. For example, when working with an individual who engages in vocal perseverations maintained by attention, a behavior analytic intervention might involve attending to the first statement while ignoring repetitive statements and providing attention for novel topics of conversation instead. However, in light of a co-occurring anxiety disorder, the initial behavior analytic approach is now contraindicated as ignoring requests will likely increase behavioral symptoms of anxiety. The intervention must be altered to account for the individual as a whole. Such changes might include neutral schedule reviews for repeated statements around upcoming events and high-quality interactions for novel topics of conversation.
Implementing Interventions with Integrity
Once the intervention is designed, implementation must include a comprehensive training plan so that all behavior-change agents (e.g., teachers, parents, therapists) understand the interaction between intervention components. That is, how each aspect of the plan works together to treat the individual as a whole. For example, an individual diagnosed with an anxiety disorder and ASD may be prescribed medication to reduce the symptoms of anxiety in general and behavioral interventions may include specific antecedent strategies to reduce the impact of certain environmental events on behavioral symptoms of anxiety such as advanced noticed for changes in schedules. Caregiver understanding of the interaction between these interventions is critical to the efficacy of implementation and thus the outcome of the intervention plan
Although not necessary, when possible, components of a multidisciplinary intervention should be implemented systematically to allow for evaluation of the efficacy of each. For example, working in concert with prescribing professionals, such as psychiatrists or neurologists, is incredibly beneficial when designing treatment packages that might be affected by prescribed medication (Newhouse-Oisten et al., 2017). For instance, some seizure medications also function as mood stabilizers and might influence behavioral interventions, making collaborating even more important. Behavior analysts should work with prescribing professionals to collect relevant measures throughout intervention and systematically change a single medication or behavioral component at a time while holding others constant. This type of ongoing collaboration across disciplines allows for systematic intervention evaluation, taking the whole person into account.
Monitoring: The Cycle of Intervention Design, Implementation, and Modification
The intervention process is not complete once the intervention is implemented. Rather, collaborative communication and monitoring are necessary to inform intervention refinements, maintenance of intervention effects, and fading in some cases. Effective, ongoing collaboration across professionals requires using common language and understandable data (Bowman et al., 2021). Behavior analysts can contribute through measurement systems that highlight correlations between variables relevant to co-occurring diagnoses (e.g., behavioral data, bowel movements, sleep patterns). For example, interventions that target toilet training for an individual with ASD and a GI diagnosis might include data collection specific to the frequency, type, and timing of bowel movements as well as prompted and independent requests for the bathroom. To best evaluate interventions targeting perseverative speech related to an anxiety diagnosis, data collection might include the frequency of perseverative speech as it relates to the timing of both environmental events and the administration of anxiety-reducing medication. It is also important to consider the individual’s engagement in their daily activities, and overall quality of life measures.
Conclusions
When it comes to assessing and treating behavior in the context of co-occurring conditions, collaboration is an essential component for achieving best outcomes for the individual. The possibility for collaboration with other fields is inherently built into some service delivery models for those with developmental disabilities, such as special education schools or behavioral units partnered with medical centers. We understand this is not the case for all behavior analysts or professionals working with individuals with ASD and co-occurring conditions. In these cases, we encourage communication across professionals to whatever extent possible by requesting individuals or caregivers seek assessment by other professionals (e.g., medical, dental, neurological), share relevant data with other service providers, and advocate for additional services relevant to co-occurring conditions when appropriate. The behavior analyst must go beyond the collection of data and ensure that the data are accessible to all members of the interdisciplinary team and the team as a whole review the data to make collaborative, data-based decisions.
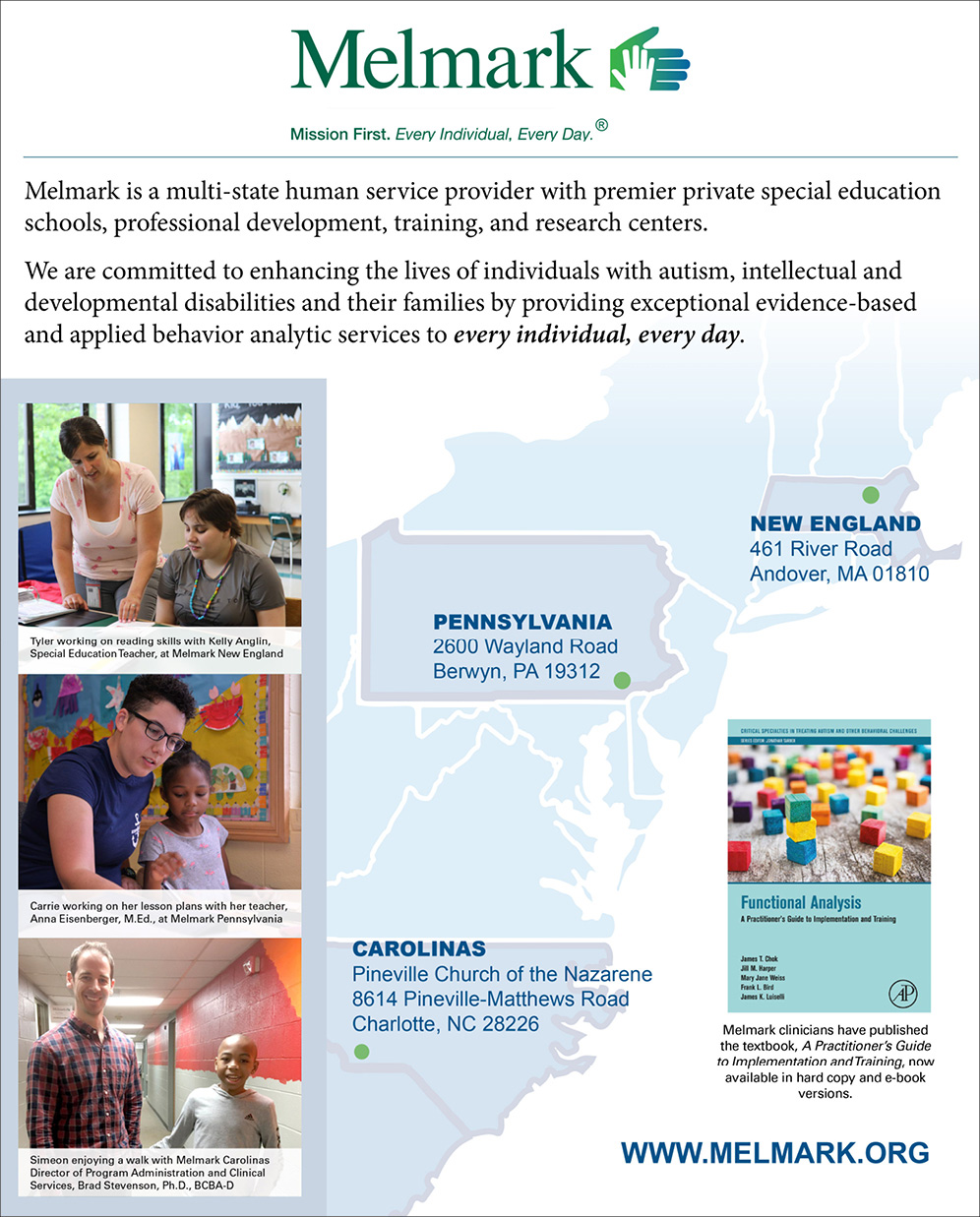
Haley M. K. Steinhauser, PhD, BCBA-D, LABA, is Director of Clinical Services at Melmark New England. Sheila A. Klick, MEd, BCBA, is a consultant at Melmark Pennsylvania. Jill M. Harper, PhD, BCBA-D, LABA, is Senior Director of Professional Development, Clinical Training, and Research at Melmark New England. Kylee A. Formento, MA, BCBA; Director of Children’s Clinical Services at Melmark Pennsylvania.
References
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). https://doi.org/10.1176/appi.books.9780890425596
Autism Speaks. (2017). Autism and Health: A special report by Autism Speaks. https://www.autismspeaks.org/sites/default/files/2018-09/autism-and-health-report.pdf
Behavior Analyst Certification Board. (2020). Ethics code for behavior analysts. https://bacb.com/wp-content/ethics-code-for-behavior-analysts/
Bird, F., Harper, J. M., Luiselli, J. K., Shlesinger, A., & Gold, J. (2022). Psychotropic medication monitoring in a human services organization for children with autism spectrum disorder: Description and evaluation of interdisciplinary team review. Behavior Analysis in Practice. Advance online publication. https://doi.org/10.1007/s40617-022-00699-4
Bowman, K. S., Suarez, V. D., & Weiss, M. J. (2021). Standards for interprofessional collaboration in the treatment of individuals with autism. Behavior Analysis in Practice, 14(4), 1191-1208. https://doi.org/10.1007/s40617-021-00560-0
Brodhead, M. T. (2015). Maintaining professional relationships in an interdisciplinary setting: Strategies for navigating nonbehavioral treatment recommendations for individuals with autism. Behavior Analysis in Practice, 8, 70-78. https://doi.org/10.1007/s40617-015-0042-7
Carr, E. G., Newsom, C. D., & Binkoff, J. A. (1976). Stimulus control of self-destructive behavior in a psychotic child. Journal of Abnormal Child Psychology, 4(2), 139-153. https://doi.org/10.1007/BF00916518
Chok, J. T., & Koesler, B. (2014). Distinguishing obsessive-compulsive behavior from stereotypy: A preliminary investigation. Behavior Modification, 38(3), 344-373. https://doi.org/10.1177/0145445513509475
Cox, D. J. (2012). From interdisciplinary to integrated care of the child with autism: The essential role for a code of ethics. Journal of Autism and Developmental Disorders, 42(12), 2729-2738. https://doi.org/10.1007/s10803-012-1530-z
Gal, E., & Dyck, M. J. (2009). Stereotyped movements among children who are visually impaired. Journal of visual impairment & blindness, 103(11), 754-765. https://doi.org/10.1177/0145482X0910301105
Goldiamond, I. (1974). Toward a constructional approach to social problems: ethical and constitutional issues raised by applied behavior analysis. Behaviorism, 2(1), 1-84.
Moore, K., Bullard, A., Sweetman, G., & Ahearn, W. H. (2021). Assessing and Treating Anxiety in Individuals with Autism. Behavior Modification. Advanced online publication. https://doi.org/10.1177/01454455211051678
Molloy, A., & Rowe, F. J. (2011). Manneristic behaviors of visually impaired children. Strabismus, 19(3), 77-84. https://doi.org/10.3109/09273972.2011.600417
Newhouse-Oisten, M. K., Peck, K. M., Conway, A. A., & Frieder, J. E. (2017). Ethical considerations for interdisciplinary collaboration with prescribing professionals. Behavior Analysis in Practice, 10(2), 145-153. https://doi.org/10.1007/s40617-017-0184-x
Rapp, J. T., & Vollmer, T. R. (2005). Stereotypy I: A review of behavioral assessment and treatment. Research in Developmental Disabilities, 26(6), 527–547. https://doi.org/10.1016/j.ridd.2004.11.005
Singer, I., Ivy, S. E., & Myers, S. (2021). Reducing stereotypies for a Student with Deaf-blindness. Journal of Visual Impairment & Blindness, 115(4), 286-298. https://doi.org/10.1177/0145482X211027502
Vollmer, T. R. (1994). The concept of automatic reinforcement: Implications for behavioral research in developmental disabilities. Research in Developmental Disabilities, 15(3), 187–207. https://doi.org/10.1016/0891-4222(94)90011-6
Walz, N. C., & Benson, B. A. (2002). Behavioral phenotypes in children with Down syndrome, Prader-Willi syndrome, or Angelman syndrome. Journal of Developmental and Physical Disabilities, 14(4), 307-321. https://doi.org/10.1023/A:1020326701399