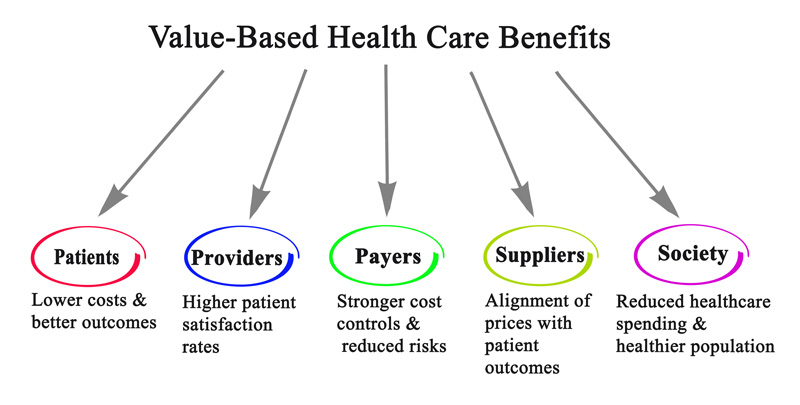
There’s a fundamental truth that often gets lost amid the complexities of behavioral health insurance costs: the paramount importance of outcomes. The call for value-based care across all healthcare is becoming louder, signaling a desire to shift from the traditional fee-for-service model to one centered on results. With the increasing rates of autism, that transformation is critical in the behavioral health space, where rising costs and fragmented care underscore the urgent need for innovation.
Catalight has been working under a pioneering value-based care system in partnership with its largest payer since 2018. Through extensive research and a decade’s worth of evidence-based practice, our clinical team is strong in the belief that lower hours of applied behavioral analysis (ABA) – especially in the form of parent-mediated care – is just as effective if not more so, than the standard, high-hour ABA.
Value-based developmental disability care redefines success not by the volume of services rendered but by the quality of outcomes achieved. It’s a departure from the unsubstantiated notion that more equals better, instead focusing on what truly matters: improving the lives of clients and their families. Catalight’s core ‘value’ is creating greater wellbeing. We’re able to create that value in as few as 8 hours a week in ABA compared to standard models that call for more than 30. Shifting to customized care presents hope for tackling the burgeoning crisis of escalating costs in behavioral health.
The biggest factor in implementing value-based care is innovation. Led by clinical indication, Catalight has been relentlessly looking at the situation differently.
Intellectual and developmental disability care defies the standardized treatment approaches all too common in fee-for-service models. Our mentality is “one size doesn’t fit all.” We fully embrace that each person we serve is unique with differing family dynamics; put together, the population, as a whole, is drastically more heterogeneous than it was when high-hour ABA became the standard in 1987. By tailoring treatment options for each client and giving choices, we seek to provide flexibility and freedom to families. When children achieve greater wellbeing through lower-hour ABA and telehealth options, parents are able to use that time for the betterment of their family wholistically – enhancing the quality of life for all members. We’re looking to do more than just deliver care – we’re reimagining it for efficiency and effectiveness.
Giving a choice in one’s care is important not only to achieve outcomes faster, which is a critical component of succeeding within a value-based environment, but also to eliminate waste and inefficiency. When there’s wasteful spending, families lose.
Catalight published a study in March that noted a diminishing return after 15 hours per week of ABA. In the fee-for-service system, more hours billed means more reimbursement without a cap or financial reason not to provide more care. Families are paying out of pocket for unneeded hours. In turn, it’s costing insurers more to cover the cost of behavioral health benefits – forcing them to increase premiums.
When treatment is more efficient with far fewer hours, not only is a family saving time that can be spent elsewhere, but they’re saving tangible dollars in cost share. By prioritizing outcomes over sheer volume, payers in value-based care are demonstrating this model is not just a theoretical concept but a pragmatic solution with proven benefits.
Payer motivation remains the chief hurdle to greater adoption of value-based care in behavioral health. Billing systems, authorization for services, and general 5-year plans are all built around fee-for-service. A transition to a value-based model requires a concerted effort to recalibrate incentives and align interests toward the shared goal of improving patient outcomes.
While such a long-term change will be complicated and arduous, the benefits to families and the behavioral healthcare industry could be monumental.
At the heart of value-based care lies a commitment to the client experience. It’s about empowering families with choice, flexibility, and convenience while sparing them from unnecessary burdens of time, stress, and financial strain. By streamlining care delivery and eliminating wasteful spending, value-based models offer a lifeline to families.
As healthcare costs spiral out of control, the need for sustainable solutions becomes increasingly more pressing. By embracing value-based care, we’re not just reimagining behavioral healthcare; we’re reshaping lives, one outcome at a time.
Trent Iden is Chief Growth Officer at Catalight, a nonprofit that provides access to innovative, individualized care services, clinical research, and advocacy – so people with developmental disabilities can choose their path. Samelson is a licensed clinical psychologist and leads the organization’s behavioral health research team with a focus on promoting the overall wellbeing of families.