Picky eating is common for children with autism spectrum disorder (ASD). Autistic individuals often show atypical eating patterns and have more difficulty with mealtime behaviors in comparison to their non-autistic peers (Christensen et al., 2019; Mayes & Zickgraf, 2019; Sharp et al., 2013). Parents of autistic youth commonly report struggles with their child’s mealtime behaviors, ranging from extreme pickiness in accepted foods to an inability to sit at the table and independently eat without distractions (Strand, 2021; Vissoker et al., 2015). Feeding challenges have co-occurred with autism for as long as autism has been recognized in the Diagnostic and Statistical Manual (Kanner, 1943; Ritvo & Freeman, 1977) and in recent years has gained an increased understanding, which has led to improved treatment options and outcomes (Christensen et al., 2019; Mayes & Zickgraf, 2019; Sharp et al., 2013). Treating feeding challenges in autistic children is multifaceted and requires a comprehensive evaluation followed by a combination of individual therapy and caregiver training (Smith et al., 2020; Zimmer et al., 2012, Zulkifli et al., 2022).
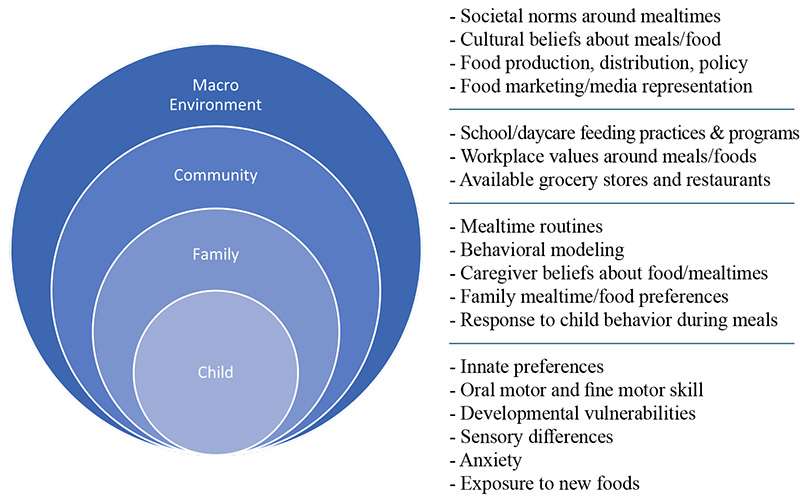
Figure 1: Multisystemic factors that influence eating and mealtime behaviors
The most common eating challenges experienced by autistic children include limited variety in accepted foods, strong preferences for certain food brands, and hypersensitivity to food textures and colors (Mayes & Zickgraf, 2019; Strand, 2021). While these are quotidian challenges for young children (Bourne et al., 2022), autistic children are more likely to develop long term rigidities around food (Strand, 2021), which can lead to nutritional inadequacies (Sharp et al., 2018) and limit a child’s capacity to participate in social engagements involving food (Kuschner et al., 2017). Multifactorial aspects of a child’s behavior, social cognition, and environment contribute to the development of restrictive eating patterns (Vissoker et al., 2015).
Core autism traits, including sensitivity to sensory input, proclivity for sameness and routines, and strong reactions to novelty, set the stage for autistic children to develop strong food preferences (Kuschner et al., 2017). Common social behavior during mealtimes, such as trying a new food to be polite, is less saliant to an autistic child due to differences in the way they process social information. Anxiety related to novel or nonpreferred foods and associated avoidance behaviors (Kuschner et al., 2017) can easily develop, including crying, spitting, gagging, eloping from the table, and aggressive behavior.
Similarly, caregivers may try to avoid children’s emotional-behavioral escalation during mealtimes, and ensure their child is getting enough calories, by accomdating their child’s preferences. Caregivers often find themselves making children their own meal separate from the family meal, allowing less nutritive foods during meals, allowing the child to wander while eating, and allowing screen use for the duration of the meal. In the long term, this pattern of child and caregiver behaviors contributes to a more limited diet and an increase in mealtime behavior problems.
Chronic restrictive eating may reach clinical thresholds for a diagnosis of a feeding disorder requiring intervention. Avoidant Restrictive Food Intake Disorder (ARFID) is a pattern of feeding disturbances in which a child exhibits a persistent lack of interest in food and habitually avoids nonpreferred food (American Psychiatric Association [APA], 2013). A diagnosis of ARFID requires persistent failure to meet appropriate nutritional needs and is associated with one, or more, of the following:
- Significant weight loss;
- Significant nutritional deficiency;
- Dependence on enteral feeding or nutritional supplements and/or;
- Marked inference with psychological functioning (APA, 2013).
Evaluating ARFID requires comprehensive, multidisciplinary assessment. Pediatricians and/or gastroenterologists are key in ruling out medical causes of feeding problems, such as reflux, constipation, food allergies, motility problems, or other chronic health conditions. Occupational therapists (OTs) evaluate sensory aspects of feeding, such as how children process the way foods look, smell, feel, and taste. Speech-language pathologists (SLPs) assess oral-motor skill development necessary for chewing and swallowing. Registered dietitians (RDs) survey nutritional status and develop dietary plans. Psychologists and other behavior health providers evaluate environmental, behavioral, and emotional factors affecting mealtimes (Smith et al., 2020; Zimmer et al., 2012, Zulkifli et al., 2022).
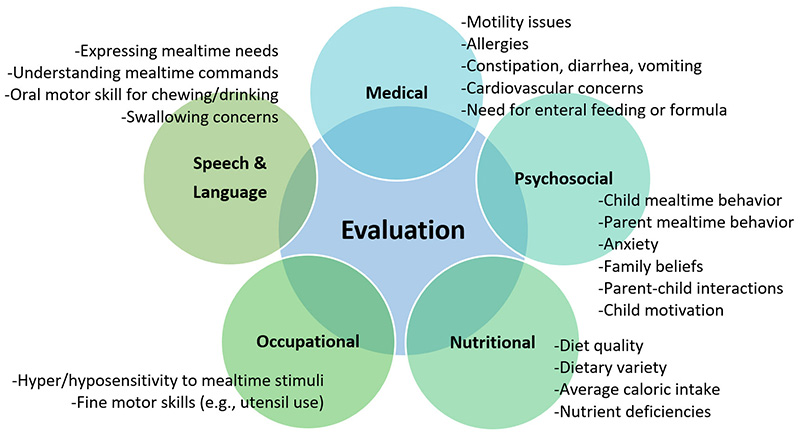
Figure 2: Multidisciplinary Components of a Comprehensive Evaluation for Restrictive Eating
Depending on the child’s age and complexity of medical, behavioral, and environmental factors, a variety of treatment options for ARFID are available. Most commonly, individual therapy with the child and coordinated training with a caregiver is indicated. Children learn the skills needed to accept new foods, while caregivers learn new strategies to support children’s mealtime behavior and expand the range of foods accepted.
Behavioral treatment can be applied in intensive form, through partial or full hospitalization programs, or in a less intensive outpatient setting. In the latter, caregivers are heavily involved in sessions to ensure carryover of skills to mealtimes at home. Behavioral strategies reduce challenging behaviors and increase food acceptance in individuals with ASD (Johnson et al, 2019). Antecedent strategies can include increasing mealtime structure, establishing discriminant stimuli through visual aids, reinforcement systems (e.g., contingent token systems, noncontingent praise, differential attention), and extinction protocols (e.g., nonremoval of spoon). These techniques in combination with rewards, planned ignoring, and escape-extinction have strong empirical support (Sarcia, 2020; Williams et al., 2010).
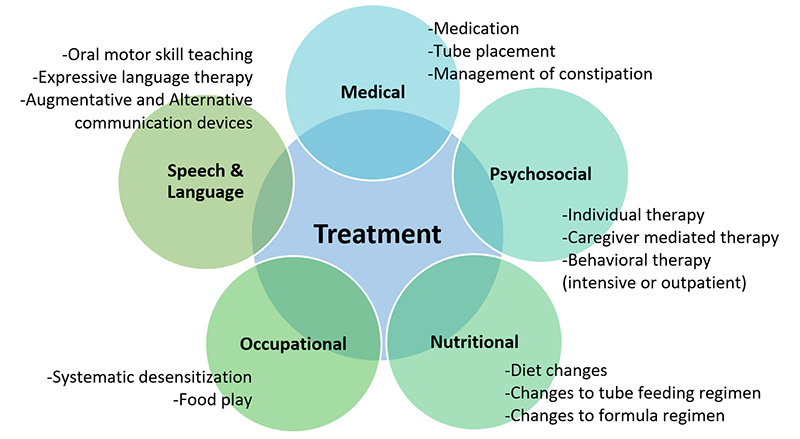
Figure 3: Multidisciplinary Components of Comprehensive Treatment for Restrictive Eating
Outpatient behavioral treatment with integrated caregiver-mediated interventions can support food flexibility by modifying caregiver responses to children’s behavior. Specifically, caregivers learn to reduce accommodation behaviors and increase supportive responses to their child (Bloomfield et al., 2019; Shimshoni, Silverman, & Lebowitz, 2020). The Autism MEAL Plan (Sharp et al., 2014) and the Behavioral Parent Training Program for Feeding Problems (Johnson et al., 2015) are two group-based programs designed to teach caregivers to address feeding problems in young (under 8 years) autistic children. In both programs, caregivers are trained in basic behavioral principles (e.g., antecedents and consequences, daily schedules and mealtime routines, effective communication, stimulus fading, shaping new feeding behaviors, and behavior tracking), then skills are applied to mealtimes to reduce behavioral challenges and increase food acceptance.
School-aged children and adolescents with ASD and ARFID can also benefit from individual and/or family-based cognitive behavioral therapy (CBT). Burton and colleagues (2021) found a combination of evidence-based treatments, Family Based Treatment (FBT) and the Unified Protocol (UP) for ARFID, effectively reduced mealtime anxiety and increased oral intake in autistic youth with ARFID. Similarly, Kuschner and colleagues (2017) piloted The Building Up Food Flexibility and Exposure Treatment (BUFFET) program as an outpatient group intervention to help autistic children aged 8-12 think and act more flexibly around food. BUFFET draws strategies from empirically supported CBT programs for autistic youth (Facing Your Fears and Unstuck and On Target). In this approach, families are first educated about malnutrition, ARFID, and strategies to enhance youth motivation to participate in meals. Then, youth and caregivers receive training in the thought-feeling-behavior connection, cognitive reappraisal, and positive behavior supports. Finally, children, caregivers, and clinicians work together to complete mealtime exposures with novel foods; children are coached to restructure negative thoughts about food and caregivers are coached to replace maladaptive parenting behaviors.
In sum, eating is a routine daily event and the behavioral and emotional difficulties associated with ARFID can create chronic distress in youth and their families. However, evidenced-based intervention is available. When consistent treatment is provided across settings, families can learn the skills necessary to shape greater food flexibility, increased oral intake, consistent mealtime routines, and a more positive mealtime environment. The key to improving feeding, particularly in autistic youth, lies in early identification and comprehensive evaluation to create a specialized treatment program that addresses the multifaceted feeding needs of the child and family.
Alana Telesford, PhD, is a licensed clinical psychologist who specializes in the evaluation and treatment of autism and feeding disorders. Shannon Santoro, MS, is an advanced extern, and Cynthia Martin, PsyD, is a clinical psychologist and director of the Autism Center at the Child Mind Institute. To learn more about the Autism Center at the Child Mind Institute, visit https://childmind.org/care/areas-of-expertise/autism-clinical-center/.
References
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.).
Bloomfield, B. S., Fischer, A. J., Clark, R. R., & Dove, M. B. (2019). Treatment of food selectivity in a child with avoidant/restrictive food intake disorder through parent teleconsultation. Behavior analysis in practice, 12(1), 33-43.
Bourne, L., Mandy, W., & Bryant‐Waugh, R. (2022). Avoidant/restrictive food intake disorder and severe food selectivity in children and young people with autism: A scoping review. Developmental Medicine & Child Neurology, 64, 691-699.
Burton, C., Allan, E., Eckhardt, S., Le Grange, D., Ehrenreich-May, J., Singh, M., & Dimitropoulos, G. (2021). Case presentations combining family-based treatment with the unified protocols for transdiagnostic treatment of emotional disorders in children and adolescents for comorbid avoidant restrictive food intake disorder and autism spectrum disorder. Journal of the Canadian Academy of Child and Adolescent Psychiatry, 30(4), 280.
Christensen, S. S., Bentz, M., Clemmensen, L., Strandberg‐Larsen, K., & Olsen, E. M. (2019). Disordered eating behaviours and autistic traits—Are there any associations in nonclinical populations? A systematic review. European Eating Disorders Review, 27(1), 8-23.
Johnson, C. R., Foldes, E., DeMand, A., & Brooks, M. M. (2015). Behavioral parent training to address feeding problems in children with autism spectrum disorder: A pilot trial. Journal of Developmental and Physical Disabilities, 27(5), 591-607.
Johnson, C. R., Brown, K., Hyman, S. L., Brooks, M. M., Aponte, C., Levato, L., … & Smith, T. (2019). Parent training for feeding problems in children with autism spectrum disorder: Initial randomized trial. Journal of Pediatric Psychology, 44(2), 164-175.
Kanner, L. (1943). Autistic disturbances of affective contact. Nervous Child, 2, 217–250.
King, H., Howarth, R., Choi, S. R., & Fischer, A. J. (2022). Using a Teleconsultation-Enhanced Treatment for Avoidant/Restrictive Food Intake Disorder in an Adolescent Male. Child & Family Behavior Therapy, 1-25.
Kuschner, E. S., Morton, H. E., Maddox, B. B., de Marchena, A., Anthony, L. G., & Reaven, J. (2017). The BUFFET program: Development of a cognitive behavioral treatment for selective eating in youth with autism spectrum disorder. Clinical Child and Family Psychology Review, 20(4), 403-421.
Mayes, S. D., & Zickgraf, H. (2019). Atypical eating behaviors in children and adolescents with autism, ADHD, other disorders, and typical development. Research in Autism Spectrum Disorders, 64, 76-83.
Ritvo, E. R., & Freeman, B. J. (1977). National Society for Autistic Children definition of the syndrome of autism. Journal of Pediatric Psychology, 2(4), 146-148.
Sarcia, B. (2020). The impact of applied behavior analysis to address mealtime behaviors of concern among individuals with autism spectrum disorder. Child and Adolescent Psychiatric Clinics, 29(3), 515-525.
Sharp, W. G., Berry, R. C., McCracken, C., Nuhu, N. N., Marvel, E., Saulnier, C. A., … & Jaquess, D. L. (2013). Feeding problems and nutrient intake in children with autism spectrum disorders: a meta-analysis and comprehensive review of the literature. Journal of autism and developmental disorders, 43(9), 2159-2173.
Sharp, W. G., Burrell, T. L., & Jaquess, D. L. (2014). The Autism MEAL Plan: A parent-training curriculum to manage eating aversions and low intake among children with autism. Autism, 18(6), 712-722.
Shimshoni, Y., Silverman, W. K., & Lebowitz, E. R. (2020). SPACE‐ARFID: A pilot trial of a novel parent‐based treatment for avoidant/restrictive food intake disorder. International Journal of Eating Disorders, 53(10), 1623-1635.
Smith, B., Rogers, S. L., Blissett, J., & Ludlow, A. K. (2020). The relationship between sensory sensitivity, food fussiness and food preferences in children with neurodevelopmental disorders. Appetite, 150, 104643.
Strand, M. (2021). Eggs, sugar, grated bones: colour-based food preferences in autism, eating disorders, and beyond. Medical Humanities, 47(1), 87-94.
Vissoker, R. E., Latzer, Y., & Gal, E. (2015). Eating and feeding problems and gastrointestinal dysfunction in Autism Spectrum Disorders. Research in Autism Spectrum Disorders, 12, 10-21.
Williams, K. E., & Seiverling, L. (2010). Eating problems in children with autism spectrum disorders. Topics in Clinical Nutrition, 25(1), 27-37.
Zimmer, M. H., Hart, L. C., Manning-Courtney, P., Murray, D. S., Bing, N. M., & Summer, S. (2012). Food variety as a predictor of nutritional status among children with autism. Journal of Autism and Developmental Disorders, 42(4), 549-556.
Zulkifli, M. N., Kadar, M., Fenech, M., & Hamzaid, N. H. (2022). Interrelation of food selectivity, oral sensory sensitivity, and nutrient intake in children with autism spectrum disorder: A scoping review. Research in Autism Spectrum Disorders, 93, 101928.








[…] [44] – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7504729/ [45] – https://autismspectrumnews.org/evaluating-and-treating-restrictive-eating-in-children-with-autism/ [46] – https://www.cvlighthouse.com/nutrition-tips-for-kids-with-autism-best-aba-therapy [47] […]