The topic of hormonal influences on women with autism has received scant attention from health care researchers. The responses to hormonal fluctuations and/or depletion of estrogen are varied and present challenges in health care prevention and promotion for some women with autism. Treatment decisions for Premenstrual Syndrome (PMS), Premenstrual Dysphoric Disorder (PMDD), Perimenopause, and Menopause can be controversial and complex. Women with autism are at risk for being excluded from this decision-making process.

Behavioral disturbances before or during menses are a frequent presenting problem in gynecological referrals for women with autism. Several reports/case studies identify marked changes related to menarche (the onset of menses) and menstruation in girls and women with autism (the majority having additional intellectual disabilities): These studies describe cyclical self-injurious behaviors (Lee 2004); an amplification of symptoms associated with autism such as sensory issues, repetitive behaviors, (Hamilton et al. 2011; Lee 2004); and mood symptoms/emotional dysregulation (Hamilton et al 2011; Obaydi & Puri 2008; Lee 2004). Oftentimes, psychotropic medications are prescribed without an adequate investigation of the cyclical nature of these behavioral patterns.
The condition known as PMS and its more severe form PMDD are often not addressed. PMS and PMDD are characterized by two key elements: symptoms (which can differ among women), and their timing in relation to the menstrual cycle.
The cyclical nature and the timing of symptoms are the central distinguishing features of these menstrual-related disorders. In the most typical pattern, symptoms begin one to ten days before menstruation and continue until after the onset of menses. In other cases, symptoms begin just after ovulation and continue until near the end of the period.
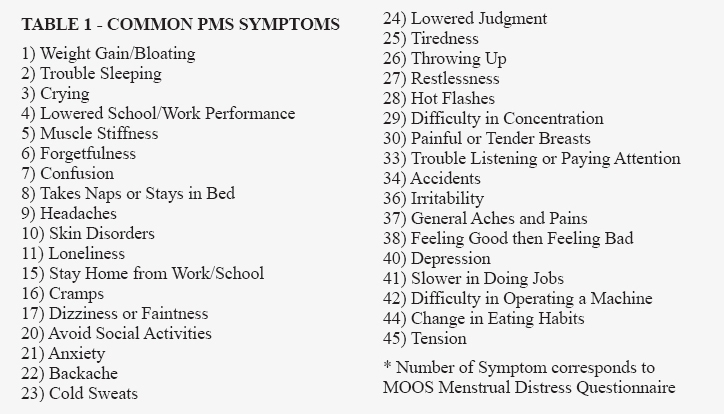
PMDD is a classification of mental disorders described in the Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5). PMS has been associated with dozens of different symptoms, though some are seen more frequently than others. Existing health problems are reported to worsen in this premenstrual (luteal) phase of the cycle. Examples common to women with autism are epilepsy, asthma, sinusitis, and chronic depression (see Table 1).
As there are no specific tests for the diagnosis of PMS, monthly charts illustrating occurrence of symptoms are necessary to diagnose the syndrome. Documenting signs and symptoms of PMS can present a challenge for health care providers of women with developmental disabilities. Often the history is either unobtainable or incomplete. PMS Assessment is best approached when charting of symptoms daily consistently occurs over a three-month interval. Bergen’s Promise, a care management organization within the New Jersey Children’ System of Care, serves a large population of individuals with autism. Through an integrated pediatric behavioral health home, the organization utilizes menstrual tracking tools, adapted from the Managing Menstruation resource from the Queensland Centre for Intellectual and Developmental Disability (Taylor, Carlson, Griffin, & Wilson, 2010), to encourage consistent charting.
Those who experience PMS often have symptoms which are typically associated with hypoglycemia, such as headaches, sweating, fainting and dizziness. These women frequently binge or crave chocolate and salty foods such as potato chips.
Women with autism PMS or PMDD may experience a symptom-free interval characterized by tremendous amounts of energy followed by a low energy time interval: relaxation and regular exercise are a must.
As women with autism age, hormonal fluctuations can impact physiological, psychological/behavioral, and cognitive dimensions of wellbeing. The transition to menopause can be divided into three phases: Premenopause, Perimenopause, and Postmenopause.
In Premenopause, hormonal fluctuations become more pronounced although the cycles remain regular. As there is a decrease in serotonin and endorphin withdrawal, menstrual migraines and mood changes become more evident. Insulin sensitivity brings on food cravings and appetite changes. If a woman with autism experiences PMS symptoms these will become more severe. Water retention, GI symptoms, breast tenderness, and heart palpitations may also occur.
In Perimenopause, the hormones of estrogen and progesterone decrease with a subsequent change in the length of the cycle and change in monthly flow. There is a further decrease in serotonin, endorphins, dopamine and estrogen brain receptors resulting in mood changes, headaches, insomnia, fatigue, and forgetfulness.
Insulin sensitivity continues to enhance food cravings and appetite changes. There is also a decrease in thyroid activity, metabolic rate and subsequent weight gain. Hot flashes, heart palpitations, skin changes (including vaginal dryness) and formication (a sensation like insects crawling on an area of skin may occur).
In Postmenopause, the woman with autism may experience some of the same symptoms of Perimenopause but to a lesser degree. Bone loss (osteoporosis) and risk of heart attack increases in this phase. Abdominal fat and an increase in waist to hip ratio also occurs.
In general, women with autism are not adequately prepared for these menopausal phases. Menstrual knowledge is commonly addressed as a hygiene issue for this population and their caregivers. Information given by the health care provider to women with autism regarding PMS/PMDD, premenopause, perimenopause and both surgical (hysterectomy-induced) and natural menopause often is scant or non-existent. It is interesting to note that in the US, education and income level are related to the likelihood of having a hysterectomy.
This group and those helping them make decisions need to be aware of the risks and benefits of Hormone Replacement (HRT).
Now that women with autism are routinely living past menopause, this aspect of life needs to be part of the health promotion strategies for this population.
The interactions of psychological, sexual, physical, vocational and recreational decisions concerning the perimenopausal and postmenopausal phases are complex and powerful. Approaches to hormonal changes effect mental health, energy levels, the cardiovascular system, bone strength, sexuality, and potential cancer risk. It is in this context that female self-advocates and all persons involved with the health and well-being of women with autism should become aware of the effects of hormonal changes during the luteal phase of menstruation (Premenstrual Syndrome), the Premenopausal phase, the Perimenopausal phase and Postmenopausal phase. Knowledge regarding health status and disease risk during these stages is essential. Increased awareness and assessment are the first line of implementation and should be implemented to promote optimal health in the continuum of hormonal passages for all women with autism.
Jan Schlaier, EdD (c); FNP-BC, is Director of Health Services and, Jacqueline Berko, RN BSN, is a Behavioral Health Home Nurse at Bergen’s Promise. We would like to thank Dean Pastras, CEO of Bergen’s Promise, for his leadership in providing integrated healthcare to Bergen’s Promise. For more information, please visit www.bergenspromise.org.
References
American Psychiatric Association (2013). Diagnostic and statistical manual of mental disorders. Ed 5. Washington, DC American Psychiatric Association.
Hamilton A., Marshal MP., Murray PJ. (2011). Autism spectrum disorders and menstruation. Journal of Adolescent Health. pp. 49: 443-445.
Lee DO. (2004). Menstrually related self-injurious behavior in adolescents with autism. Journal of the American Academy of Child and Adolescent Psychiatry. 43: 1193.
Obaydi, Puri BK. (2008). Prevalence of premenstrual syndrome in autism: A prospective observerated study. The Journal of International Medical Research. pp. 36: 268-272.
Taylor, M., Carlson, G., Griffin, J., & Wilson, J. (2010). Managing Menstruation. Retrieved from https://qcidd.centre.uq.edu.au/files/262/Menstrual%20Management%20Booklet%202010%20in%20colour.pdf





Are there any current studies about menstruation and autism? I would be happy to know more or be a part of it. I am autistic and experience many of the above symptoms with very little help or support from Doctors. In fact I was told I must be one of the unlucky ones and that’s all the help I was given.
There is not much research on this topic available. Check out the results from this Google search for “menstruation and autism studies”: https://scholar.google.com/scholar?q=menstruation+and+autism+studies&hl=en&as_sdt=0&as_vis=1&oi=scholart
[…] Source:Autism Spectrum News […]
Hi Hayley,
I’m also autistic and have ADHD. Just like you I struggle immensely with worsening of my symptoms before my period.
I also have a histamine intolerance and several allergies (and Asthma). When I found out that all these things very often co-occur I started taking a closer look
After reading several studies (the amount of information is ridiculous low considering how many people are affected if you ask me), you could summarize my findings like this:
Inflammation appears to play a role in autism and ADHD symptoms (and how intensely they present).
2. Almost always autistic people and people with ADHD have deficiencies when it comes to certain vitamins and minerals.
With my findings I made adjustments in my diet and got my blood tested. Only after that I begun (following the discovery of several deficiencies) to supplement. To blindly supplement potential deficiencies can be dangerous and you should always back it up with hard data first.
Also, don’t take any supplements at least a month before getting tested (as it might influence the results). Typical deficiencies with ADHD are vitamin D, iron and magnesium. I was very low on both of them (among others).
If you don’t want or can’t get your blood tested, please educate yourself online before taking anything!
Additionally, I take quercentin, vitamin C, and omega 3 oil (from algae-important is the ratio EPA to DHA, look it up!). All organic. I make sure it’s pure without any crap or vitamin’s added, I might not need.
Since trying to fix my deficiencies and taking the quercentin, vitamin c and omega 3 (which very much simplified reduces the inflammation within the body) I struggle a bit less in the days before my period.
One last tip that might sound weird: try taking antihistamines. While they only block the histamine receptors instead of really reducing the histamine in your body, taking antihistamines can bring you temporary relief (and yes, I’m talking about autistic symptoms as ridicuous as it might sound).
But please only take antihistamines occasionally. Taking antihistamines for longer periods of time can have the opposite effect.
I’m sorry for this long comment but hope I could help a bit.
Greetings from Germany!
Hi Melanie
Very interesting reading your comment . ( I’m a different Hayley btw )
Im really going through hell lately . Since having a child ( now 4) I’ve had very severe periods. Extremely painful with all of the other symptoms , swelling , moods , heightened sensitivities. Now I have bowel inflammation with has really made me ill. No diagnosis of autism yet but almost sure myself and my daughter are on the spectrum. Im also now trying vitamins to help myself as doctors just treat me like I’m an alien. Im trying cod liver oil , vit d , magnesium citrate , and vitamin k2 . Eat a good diet , make my own juices , smoothies etc. I’ve also had allergic reactions throughout life with no known cause , was diagnosed with type of angioedema in my teens. Lots of facial swelling , now my daughter is having the same and no known cause we can pinpoint. Can you contact me please if you can offer any further help or advice. I would be very interested to talk to you about this. Thankyou Hayley R
I believe I am Autistic, 2 of my children were diagnosed with Asperger’s and 1 grandchild, and another grandchild is being tested. No one will test me, though I’ve always had the same meltdowns as my daughter throughout my life, my sensor’s have always been through the roof. Hearing, smell, touch,I tend to love too deep, I tend to hurt too deep, feelings in general, social situations always made me want to run. When people ask me how my day is, I tend to tell the truth, or tell a life story, I was an honour student with marks in the 90’s until I move a few provinces away where I got picked on, teased, called names which I take seriously to heart. Now I have hit menopause. I can’t stand the smell of myself, it is so nauseating and I don’t know what to do. I need help.
[…] PMS and PMDD as well as other possible issues associated with periods. Several sources such as Autism Spectrum News and the previously mentioned journal, Autistic Experiences of Menstruation, note that […]