An estimated 5 million people in the United States are living with complex communication needs (CCN) (Beukelman & Light, 2020). This estimate includes people across all age groups and disability types who experience difficulties meeting their communication needs using only verbal speech. Alternative and augmentative communication (AAC) methods offer a way to communicate for people who do not use verbal speech or who have significant limitations on their speech. AAC may be appropriate for people of any age when they have the opportunity and support needed to learn.

Darius using his AAC device to communicate with staff
In typically developing individuals, language acquisition begins around 6 months and continues developing through early adolescence. If a child does not use functional speech by age 5, they are considered nonverbal or minimally verbal (Tager-Flusberg & Kasari, 2013). Historically, it was believed that if language skills did not develop prior to age 5, a person would be unable to gain this skill later in life. However, with the growing availability of alternative communication methods, learning to communicate does not have to be limited to young children and may be possible well into adulthood.
Many nonverbal and minimally verbal adults rely on non-symbolic communication, such as eye gaze, gestures, facial expressions, and body language, to meet their communication needs. While these methods are effective in some circumstances, non-symbolic communication significantly limits the type and variety of messages an individual can communicate. AAC increases access to symbolic communication, which consists of spoken and written language, signed languages, and picture symbols. With increased access to symbolic communication via AAC, non-verbal and minimally verbal individuals can expand their communication abilities to include more complex and abstract messages.
Why Was My Adult-Child Never Offered AAC Before?
Children with CCN have access to speech-language pathology (SLP) services up to age 21, as schools must provide a Free and Appropriate Public Education (FAPE) (Office for Civil Rights, 2010). However, access to SLP services in public schools and AAC treatment is relatively recent, with the passage of the Individuals with Disabilities Education Act (IDEA) in 1975 and the introduction of AAC as a viable treatment option in 1981 (U.S. Department of Education, 2024; Calculator & Delaney, 1986; Gorenflo & Gorenflo, 1991; Shane & Cohen, 1981).
Given this history, adults 43 or older, likely never had access to the services necessary to meet their complex communication needs. Even today, individuals leaving the public education system may not have received adequate AAC support, as knowledge of when to implement AAC and how to provide effective treatment continues to be limited (Assistive Technology Industry Association, 2011, as cited in Brittlebank & Sowers, 2024).
Although many adults with CCN may not have received AAC intervention as children, increasing meaningful communication is still possible and valuable as an adult. Melmark is a multi-disciplinary disability services agency at the forefront of supporting life-long communication opportunities for adults with disabilities. With the introduction of adult speech therapy services in 2018, 45 of Melmark’s 70 non-verbal/minimally verbal adult residential clients have gained access to functional symbolic communication through AAC. In other words, these individuals are able to use picture symbols on a device to communicate their wants, needs, and thoughts, greatly expanding their ability to effectively express themselves to others. The following case studies discuss two individuals at Melmark whose communication journeys demonstrate the value of AAC in adulthood and highlight steps and considerations when pursuing AAC for adults.
Who Could Benefit from AAC?
Even without access to verbal speech or AAC, people with CCN are often able to communicate some of their needs using non-symbolic communication, such as eye gaze, vocalizations, body movements, and physical manipulation of a person or object. AAC offers access to symbolic communication through methods other than verbal speech, which greatly expands the type and clarity of communication available to the individual. AAC is typically recommended for people who are nonspeaking, but it may also benefit people who have limited verbal output, and people with low speech intelligibility. Melmark clients Will and Darius demonstrate contrasting profiles of individuals who may benefit from AAC.
Will
Will is a nonspeaking 57-year-old man with severe intellectual disability and spastic quadriplegic cerebral palsy. He is a highly social individual who spent the majority of his life relying on non-symbolic communication. When unable to effectively express himself, Will engaged in challenging behaviors, such as disruption and aggression, in an attempt to meet his needs. Will was 51 when he first trialed AAC to support his communication.
Darius
Darius is a 38-year-old man with moderate intellectual disability, spastic diplegia with left hemiparesis, and optic neuropathy. He can communicate through vocal/verbal means, but his speech is highly unintelligible to unfamiliar listeners or in an unknown communicative context. Darius may attempt to repair communication breakdown when prompted, but most often he will change the subject or stop talking altogether. At age 32, Darius trialed articulation therapy to improve intelligibility, but he had limited success due to the severity of his deficits. He began utilizing a speech-generating device (SGD) to support his communication at age 37.
When determining who may benefit from AAC in adulthood, it may help to move away from asking, “Can this individual communicate anything?” and toward, “Can this individual communicate everything?” To narrow this broad question, consider whether an individual can engage in new environments, with new people, using the six primary functions or reasons why we communicate:
- To request – ask for what you want or need
- To protest – express dislike, disinterest, or discomfort
- To comment – identify people, things, and experiences in our environment
- To ask questions – gain information about specific topics
- To socialize – engage in greetings, gain attention, and build social closeness
- To share information – discuss your thoughts, opinions, ideas, and feelings
How Do You Choose an AAC System?
AAC is an umbrella term used to describe many different alternative communication methods. AAC is commonly subdivided into high-tech and low-tech categories. Low-tech AAC includes systems such as single-message voice output buttons, the picture exchange communication system (PECS), and picture point boards. High-tech AAC refers most commonly to speech-generating devices (SGDs), which utilize a digital display and produce a multitude of auditory messages. We will return to our case studies for examples of the AAC trial and selection process.
Will
In 2018, Will began using the Picture Exchange Communication System (PECS) – a low-tech system in which an individual gives a picture of an object to a communication partner to make a request. Initially, PECS served this client’s communication needs, as he established his understanding of symbolic communication. However, due to limited mobility, he could only communicate with people in his immediate area. Additionally, icons became lost or damaged overtime, limiting what he could communicate to what icons were available. Will showed an increase in challenging behaviors when he could not request or gain staff attention effectively using PECS, indicating the need to consider other AAC options.
In March 2023, Will began trialing a speech-generating device (SGD). The SGD provided auditory output, allowing Will to communicate with people at a greater distance. It also increased his access to vocabulary, as his communication layout could easily expand as his skills grew. During the trial period, Will demonstrated consistent interest in using the device, and he quickly began to independently activate icons on the screen to make requests. He also demonstrated skills in operating the device, independently illuminating the screen, and using arrows and folders to navigate to different vocabulary pages. After this successful trial, Will received his own SGD in April 2023.
Darius
In February 2023, Darius began trialing a high-tech SGD to support his verbal communication when communication breakdowns occurred. Due to his significant visual impairment and motor deficits, this client initially demonstrated difficulty navigating the flat touch-screen surface of his SGD. However, his use of the device improved with changes to the graphic display to enhance visibility, and the implementation of a keyguard – a customized plastic screen overlay – to support fine motor access. Darius’ SLP and PT team also worked together to position the device on the client’s wheelchair, allowing for improved visual and motoric access on the go.
There are pros and cons to using any AAC system. Low tech systems are easily transported and typically low-cost, offering an accessible entry point for many first time AAC users. However, they are limited in the amount of vocabulary available, and they do not offer or have very limited auditory output. High-tech systems offer flexibility in the size of the communication layout, the amount of vocabulary available, and the ease of editing and updating as communication skills change. However, these devices are often costly and require some technological knowledge to edit and operate. Selecting the right AAC system is a highly individualized process that requires trialing different systems to determine physical accessibility, the ability to meet the client’s current and future communication needs, as well as client and family preferences. When possible, it is beneficial to collaborate with an interprofessional team to select and implement an appropriate AAC device. Team members may include:
- Speech-Language Pathologists (SLPs)
- Occupational Therapists (OTs)
- Physical Therapists (PTs)
- Behavior Analysts (BCBAs)
- Residential and/or Day Program managers
How Does AAC Support Communication Skills?
Gaining access to an AAC system is only part of the equation when working to improve communication for adults with CCN. It is also essential to teach individuals how to use the device and effective methods of communicating. After selecting an AAC system for an individual, developing the skills to use the system requires continuous exposure and education. The methods for teaching an AAC system are two-fold: individualized direct treatment sessions and incidental learning in the natural environment. Individual treatment sessions target specific skills to support the user with their device and communication development. The skill areas focused on in treatment follow the communicative competencies outlined by Janice Light (1989; Light & McNaughton, 2014), specifically:
Linguistic Competence: language skills such as vocabulary and grammar
- Examples: requesting, labeling, building multi-word sentences
Operational Competence: technical skills related to the AAC system
- Examples: navigating folders/pages, activating and clearing the message bar, navigating the environment with an AAC system
Social Competence: skills for social engagement using AAC
- Examples: taking conversational turns, appropriately entering/exiting a conversation, topic maintenance
Strategic Competence: compensatory skills for repairing communication breakdown
- Examples: repeating a message, gaining the conversational floor (e.g., “please, wait for my message”)
Psychosocial Competence: skills related to motivation to communicate and self-confidence
- Examples: persistent communication if misunderstood, developing device ownership
During individual treatment, the communication partner contrives learning opportunities to allow for repeated practice with the targeted skills. For example, the communication partner may set up a “requesting session,” during which they offer a variety of choices for the AAC user to request for in quick succession. During such a session, the AAC user practices the vocabulary for making requests, the operational steps to access each of the vocabulary terms, and the social timing of when it is appropriate to make a new request.
Contrived treatment sessions offer opportunities for massed practice, which supports new skill acquisition. However, AAC users also benefit from natural environment teaching, in the form of modeling, to generalize new skills and support continual learning. Modeling consists of the communication partner using the AAC system to express their own message during daily routines, conversations, and activities. The following are examples of ways to model during daily routines:
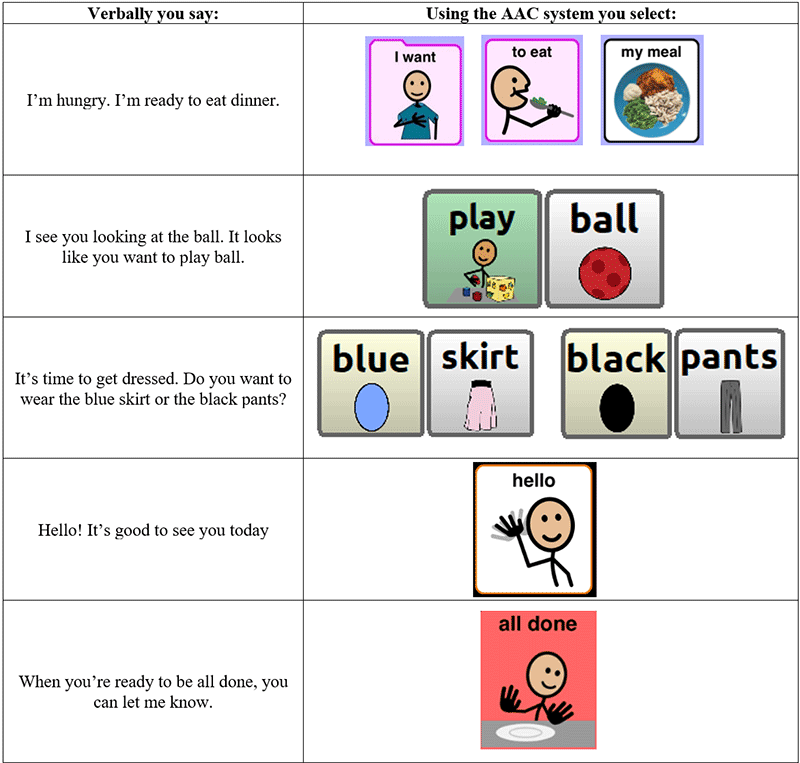
Through modeling different messages, the communication partner demonstrates the location of new vocabulary, different types of communication (e.g., commenting, labeling, social engagement), and how to navigate the AAC system. If you are unsure where to begin, some guidelines for effective modeling include:
- Use your own words – you speak through the AAC system
- No response required – the AAC user does not have to say anything back to learn from the interaction
- Lower the pressure – make statements rather than asking questions and give plenty of wait time for a response
- Engage naturally – use activities in the environment and your daily routine to start conversations
- Making mistakes is OK – even your mistakes provide valuable information about how to look for words and ways to navigate the AAC system.
At the end of the day, the only wrong way to model is by not modeling at all. Through offering frequent communication examples and adequate time to learn, you can support your adult child in improving their communication abilities. When given the necessary support, communication improvement is possible even in adulthood. Consider the outcomes of our two case studies:
Will
After 1 year with an SGD, Will has demonstrated incredible communication gains. He is capable of requesting preferred items and activities across a variety of categories, including foods, drinks, toys, and locations. He also uses functional communication responses (FCRs) to gain access to attention, leave an area, and express that he is finished with an activity. These FCRs have significantly decreased this client’s reliance on challenging behaviors to meet his needs. Lastly, given Will’s social nature, he has thrived with access to social language, which allows him to greet others, introduce himself, and identify the names and pictures of people he interacts with. Over the past year, this client has experienced age-related changes to his mobility, but his SGD has changed with him, allowing him to continue to access communication. He now uses a walker bag to safely carry the device with him, and he began using a keyguard to support his fine motor skills. During his most recent individual support plan meeting (ISP), this client demonstrated his love of his communication device, showing it off to his family and team and requesting attention from everyone in the room. At the end of the meeting, Will’s mother said “I wasn’t sure when you suggested the device. I am so pleasantly surprised that he has learned so much.”
Darius
After receiving his own SGD in March 2023, Darius developed a clear love for and ownership of his device. He is responsible for taking the device with him, and if it is not within his view, he will say “my iPad” to get help finding it. Darius can utilize his device to clarify his message when his verbal speech is not understood. He has also benefited from increased access to social and phrase-based communication. Darius enjoys exploring the names of friends and staff members, and he has been practicing using social phrases, such as “see you later alligator,” to build diversity in his verbal repertoire. Darius continues to use his verbal speech, but his SGD has increased the clarity with which he can express his thoughts and feelings.
Summary
Adults with complex communication needs can improve communication skills when given access to and instruction in AAC. Any adult who is unable to effectively communicate their wants, needs, and thoughts using verbal speech may be a candidate for an AAC system. When choosing an appropriate AAC system, you must consider the individual’s communication needs, their physical access, and for what system they demonstrate a preference. Once you have selected an AAC system, a combination of direct skill instruction and communication modeling are essential to support communication development and generalization of device use across settings and communication partners.
Readers can continue to expand their AAC knowledge or gain support during the AAC journey using the following resources.
Education and Support Resources
AbleNet: AAC Resources (Augmentative and Alternative Communication Resources)
ASHA: American Speech & Hearing Association: AAC (Augmentative and Alternative Communication)
AssistiveWare: Strategies for AAC use at Home
Easterseals: Caregiver Resources and Groups
ISAAC: International Society for AAC (International Society of Augmentative and Alternative Communication)
- USSAC: US Society for AAC (U S Society for Augmentative and Alternative Communication)
NWACS: AAC in Adults with IDD (Augmentative and Alternative Communication in Adults with Intellectual and Developmental Disabilities)
NWACS: Blog posts related to AAC for Adults with IDD (Augmentative and Alternative Communication for Adults with Intellectual and Developmental Disabilities)
PRC: Caregiver Resources
SPD: AAC for Caregivers Training & Manual (Augmentative and Alternative Communication for Caregivers Training and Manual)
Laura Nagy, MS, CCC-SLP is a Speech-Language Pathologist at Melmark.
This article has been republished with permission from the Association for Science in Autism Treatment. The original source can be viewed here
References
Beukelman, D. R., Light, J.C. (2020). Augmentative & alternative communication: Supporting children and adults with complex communication needs (5th ed.). Brookes Publishing.
Brittlebank, S., & Sowers, D. J. (2024). Developing augmentative and alternative communication competence in preservice speech-language pathologists: A collaborative model for clinical educators. American Journal of Speech-Language Pathology, 33(1). 1-15. https://pubs.asha.org/doi/full/10.1044/2023_AJSLP-23-00125
Calculator, S. N., & Delaney, D. (1986). Comparison of nonspeaking and speaking mentally retarded adults’ clarification strategies. Journal of Speech and Hearing Disorders, 51 (3). 252-259. https://pubs.asha.org/doi/10.1044/jshd.5103.252.
Gorenflo, C. W., & Gorenflo, D. W. (1991). The effects of information and augmentative communication technique on attitudes toward nonspeaking individuals. Journal of Speech and Hearing Research, 34(1). 19-26. https://doi.org/10.1044/jshr.3401.19
Light, J. (1989). Toward a definition of communicative competence for individuals using augmentative and alternative communication systems. Augmentative and Alternative Communication, 5(2). 137-144. https://doi.org/10.1080/07434618912331275126.
Light, J., & McNaughton, D. (2014) Communicative competence for individuals who require augmentative and alternative communication: A new definition for a new era of communication?, Augmentative and Alternative Communication, 30 (1). 1-18, https://doi.org/10.3109/07434618.2014.885080.
Office for Civil Rights. (2010, August). Free appropriate public education for students with disabilities: Requirements under section 504 of the Rehabilitation Act of 1973. U.S. Department of Education. https://www2.ed.gov/about/offices/list/ocr/docs/edlite-FAPE504.html.
Shane, H. C., & Cohen, C. G. (1981). A discussion of communicative strategies and patterns by nonspeaking persons. Language, Speech and Hearing Services in Schools, Volume 12(4). 205-210. https://doi.org/10.1044/0161-1461.1204.205.
Tager-Flusberg, H., & Kasari, C. (2013). Minimally verbal school-aged children with autism spectrum disorder: the neglected end of the spectrum. Autism research: Official Journal of the International Society for Autism Research, 6(6), 468–478. https://doi.org/10.1002/aur.1329.
U.S. Department of Education. (2024, February 16). A history of the individuals with disabilities education act. https://sites.ed.gov/idea/IDEA-History.





