In December 2019, the Cerebral Palsy Associations of New York State (CPNYS) partnered with StationMD, a for-profit physician service providing telemedicine to vulnerable populations, to participate in a five-year grant funded by the New York State Department of Health. The Statewide Care Facility Transformation Program grant offers a single strategy for an alternate model of care via telemedicine for more than 8000 lives.1 The Telemedicine Triage Project (TTP), as it is known, is “an innovative model that provides telemedicine consultations for people with intellectual disabilities (PIDD) who reside in state-certified group residences across the state of New York in the United States, and present with an urgent but non-emergent medical concern when their usual provider is unavailable.”1
Services for the UnderServed (S:US), located in New York City, participates in this grant program along with other provider agencies. S:US provides services for individuals, which include a comprehensive array of supports to people with life circumstances marked by intellectual/developmental disabilities (I/DD), behavioral health and substance use challenges, histories of incarceration, and trauma. S:US’ history has been about supporting people and communities that have been marginalized, communities of color, and communities impacted by poverty, homelessness, and food insecurity. This article chronicles our journey in this telemedicine program, including the impacts of health access disparities faced by people with I/DD.
The telehealth group StationMD provides specialized telemedicine clinicians to I/DD populations across 22 states. Its services include 24/7 urgent care, as well as behavioral health/psychiatry treatment for people with I/DD. StationMD’s telehealth solution has been recognized by The Center for Medicare and Medicaid Innovation as an innovative telehealth solution for the I/DD population.4 Given its expertise, StationMD was selected by CPNYS for this telehealth grant project.
The rapid adoption of telehealth services was critical during the pandemic because hospital care was only available to the very ill. “One positive outcome of the COVID-19 pandemic was that the lockdowns and physical distancing forced a pivot to telemedicine and the increased use of other technology solutions to bring support to persons with ID/DD while minimizing physical contact.”5 The timing for the rollout was concomitant to when community health access became limited. After decades of challenges and barriers to care, this organized intervention sourced between non-profit and for-profit entities created an entirely new access point.
Reflective of cultural responsiveness and emphasis on health equity, telehealth service provision of care moderates the gap of access disparity. StationMD is not a replacement for primary care physicians but provides an additional layer of immediate clinical decision-making support that can also help bridge care during off-hours, weekends, and holidays. StationMD allows for the blend of a specialized remote service linkage of care for a person supported in their home environment, surrounded by familiar staff, with the option for families to join the session.
StationMD is ramping up behavioral health services as a response to increased demand, partnering with S:US to secure community behavioral health services for people served with I/DD. “Despite the prevalence of mental health conditions, research suggests that people with IDD may not be receiving adequate mental health care in the community.”2 S:US has transitioned select individuals requiring medication stabilization to StationMD. A huge benefit of StationMD’s behavioral health services is that psychiatrists who specialize in PIDD are accessible in between scheduled appointments.
S:US program leadership staff articulated the impact, benefits, and disadvantages of telehealth services:
“I am grateful for telehealth visits as it is convenient and minimizes the long period of time that the people we serve have to wait at clinics. The disadvantage of a telehealth visit is that the medical provider has to determine a diagnosis, and oftentimes it is difficult for the medical provider to provide a thorough physical examination of the people we serve virtually.”
“I notice some staff are not tech savvy, and also, you have to worry about connecting to the internet when it’s time for the virtual appointment to be conducted.”
“I must say it is very efficient for minor conditions. Telehealth wait time is no more than three minutes.”
There can be some hesitation in navigating technology when starting to utilize a telehealth service. “When we created our process, we knew we had to keep things simple and help the patient and their caregiver connect to the doctor,” says Dr. Matthew Kaufman, CEO of StationMD. During every encounter, clients use a telephone to call a toll-free number, and a StationMD technical assistant guides the patient into a virtual visit with a specialized doctor. Kaufman continues, “After the first time the patient and their caregiver use our service, they realize how simple it is to use.”
According to Dr. Deven Unadkat, Chief Medical Officer at StationMD, clinicians are able to successfully resolve the patient’s medical issue 90% of the time during the telehealth encounter. Not all cases can be safely managed by telehealth. When conditions warrant an emergency room visit, the clinician will call the hospital emergency room and discuss the case with the receiving doctor. This streamlines the hospital visit process for clients, and pertinent clinical information is conveyed from doctor to doctor.
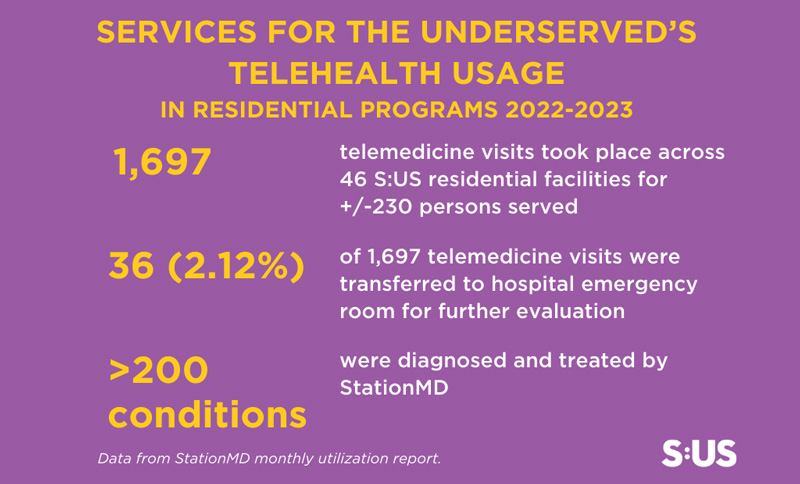
Approximately 98% of the S:US visits in 2023 resulted in effective care of PIDD in the safety of their own home. People served by S:US were able to spend more time doing the things they enjoy and less time traveling and waiting for medical care. “The American Hospital Association task force believed that virtual care strategies would allow vulnerable communities, particularly those that have difficulty recruiting or retaining an adequate health care workforce, the opportunity to maintain or supplement access to health care services.”3 S:US saved over $60,000 on direct care staff expenses over a two-year period as a direct result of utilizing StationMD services.7 Currently, there is a national Direct Support Professional (DSP) workforce shortage.6 S:US is leveraging the cost savings to provide further support for DSP recruitment and retention activities.
Due, in large part, to the pilot’s success, New York State has established permanent models for people with I/DD to receive telehealth services. For people in OPWDD-Certified group homes, the service is now an allowable cost to contribute to the rate of reimbursements by the state. For 1915c waiver recipients residing outside of certified group homes, it is expected that there will be a pathway to services under the waiver.
Telehealth has provided flexibility and a critical pipeline to the delivery of care for the I/DD population in a complex healthcare environment. Trusted partnerships, as evidenced by S:US’ collaboration with a telehealth service provider such as StationMD, are proven sustainable models and solutions to reduce pressure on care providers and the healthcare delivery system as a whole. The impact of this strategic partnership reinforces S:US’ philosophy of providing tailored, person-centered services in integrated settings to transform the lives of the people we serve and improve our communities.
Courtney Morgan, MBA, RN, is Senior Vice President, Health & Clinical Services at Services for the UnderServed (S:US). Deven Unadkat, DO, MPA, FACEP, is President at StationMD, PC and Chief Medical Officer at HealthTech Partners, Inc.
For more information about S:US’ services for people with intellectual/developmental disabilities, visit sus.org/our-services/intellectual-developmental-disabilities. For more information about StationMD, visit stationmd.com.
Footnotes
1) Berry A.C., Kwok L., Gofine M., Kaufman M., Williams AD., Terlizzi K., Alvaro M., Neighbors JC. Utilization and Staff Perspectives on an On-Demand Telemedicine Model for People with intellectual and Developmental Disabilities Who Reside in Certified Group Residences. Telemedicine Reports, 20234(1), 204-214. DOI: 10.1089/tmr.2023.0024.
2) Lineberry S., Bogenschutz M., Broda M., Parthenia D., Prohn S., West A. Co-Occurring Mental Illness and Behavioral Support Needs in Adults with Intellectual and Developmental Disabilities, Community Ment Health J, 2023 1-10 DOI: 10 1007/s10597-023-01091-4 Retrieved from ncbi.nlm.nih.gov/pmc/articles/PMC9899157.
3) Bhatt J., Bathija P. Ensuring Access to Quality Health Care in Vulnerable Communities. Academic Medicine. 2018;93(9): 1271-1275.DOI: 10.1097/ACM.0000000000002254.
4) Resources for Integrated Care. (Feb 21, 2023) People with Intellectual/Developmental Disabilities: Telehealth Overview. Resources for Plan & Providers for Medicare-Medicaid Integration. Retrieved from resourcesforintegratedcare.com/2023_brief_people_with_intellectual_developmental_disabilities_idd_telehealth_overview/.
5) Tasse M., Wagner J., Zhang, X. (2023) Ohio StationMD Pilot Program: Report on Outcomes [White paper]. Nisonger Center, Ohio State University. Retrieved from nisonger.osu.edu/research/stationmd-evaluation/.
6) Laws C. (2019) The Direct Support Professional Workforce Crisis: Challenges, State Approaches, and opportunities for Georgia [White Paper]. The University of Georgia: The Institute on Human Development and Disability. Retrieved from gcdd.org/images/public_policy/2020/White_Paper_on_the_DSP_Crisis_CBL_10042019.pdf.
7) Wicklund, E. (2023). I/DD Care Provider Uses Telehealth to Save 100K in ER costs over 2 years. HealthLeaders Media. healthleadersmedia.com/telehealth/idd-care-provider-uses-telehealth-save-100k-er-costs-over-2-years.









[…] Telehealth Service Delivery to Persons with Neurodevelopmental Disorders […]